Antibiorésistance, le combat de Michèle Rivasi (EELV) : l'Université de Tel Aviv a trouvé la parade à l'apocalypse des antibiotiques

[:fr]Non vous ne rêvez pas. L’ESCMID (Société européenne pour la microbiologie clinique et les maladies infectieuses), a récemment prédit une « Apocalypse des antibiotiques en France d’ici à 2025 avec la propagation de bactéries résistantes provenant de Grèce et d’Afrique du Nord qui pourrait provoquer un million de morts ». Alors que Michèle Rivasi (députée européenne, vice-présidente du Groupe Verts / ALE) a fait de l’antibiorésistance son cheval de bataille*, le Pr Udi Qimron de l’Université de Tel Aviv a justement mis à jour des mécanismes pour rendre les supermicrobes à nouveau sensibles aux antibiotiques. Israël Science Info souligne l’importance vitale des travaux du Pr Udi Qimron qui sont d’une portée universelle.
Selon des prévisions, les infections bactériennes dues à ces microbes superrésistants, tueront d’ici quelques décennies plus que le cancer et pourraient coûter la bagatelle de 100 milliards de dollars par an. Pour la revue britannique « review on antimicrobial resistance », ces superbactéries seraient d’ores et déjà responsables de 700 000 décès par an. L’utilisation larga manu des antibiotiques, chez l’homme et surtout chez l’animal, a contribué à développer des résistances à ces médicaments. Il faut alors recourir à des doses plus importantes ou associer plusieurs thérapies pour éradiquer certains micro-organismes. Cette évolution est très préoccupante. Le risque est l’émergence de bactéries « superésistantes », capables de survivre à tout type de traitement antibiotique. Or, la recherche n’a pas mis à jour ces dernières décennies de nouveaux antibiotiques, ni de nouvelles stratégies pour lutter contre les infections bactériennes. Dans le combat de l’homme contre le microbe, ce dernier a donc pris une longueur d’avance. Lors de sa dernière Assemblée générale à Genève en juin 2015, l’OMS a appelé à un plan mondial pour freiner ces problèmes d’antibiorésistance et ouvrir le chemin à de nouvelles approches. C’est précisément à cette exigence cruciale que répondent les travaux remarquablement innovants de l’équipe du Pr Udi Qimron, à l’université de Tel Aviv (Dr Ido Yosef, avec Ruth Kiro et Shahar Molshanski-Mor, doctorants au département d’immunologie et de microbiologie cliniques) et de deux scientifiques américains, le Dr Sara L. Milam et le Pr Harold P. Erickson, de la Duke University Medical Center. Ces recherches menées depuis plusieurs années portent sur la possibilité de rendre les bactéries résistantes à nouveau sensibles aux antibiotiques.
Un voyage dans le temps
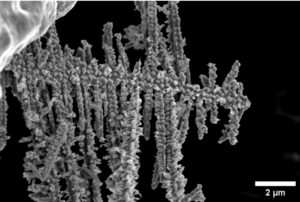
En d’autres termes, de les faire « revenir en arrière ». Les premiers résultats de ces travaux sont très prometteurs. Parce que les bactéries et les virus ont évolué conjointement pendant des millions d’années, le Pr Qimron a eu l’idée que les virus pouvaient contenir des armes essentielles à la destruction des bactéries. L’équipe du Pr Qimron s’est intéressée à des virus particuliers les phages (ou bactériophages). Ces virus infectent les bactéries et s’y répliquent. Comme tout virus infectant une cellule, le phage s’attaque à l’ADN du noyau de la cellule qu’il infeste et le modifie. Ces phages sont extrêmement nombreux à la surface de la terre et on estime qu’ils existent dans une proportion de 10 pour une bactérie. « Deux ans et demi de recherche ont été nécessaires pour étudier les 56 protéines d’un virus qui infecte une bactérie puis à localiser les mutations des gènes qui aident la bactérie à résister à la toxicité des protéines produites par le virus. Grâce à des techniques de séquençage à haut débit de l’ADN, les chercheurs ont identifié une nouvelle petite protéine (Gp 0,6) qui inhibe une autre protéine nécessaire à la survie de la bactérie« , commente le Dr Sivan Cohen Wiesenfeld, rédactrice de recherche pour l’Université de Tel Aviv et membre du comité scientifique d’Israël Science Info. L’étude portait sur certains types de bactéries (escherichia coli) et donc certains phages spécifiques à ces bactéries (E coli phage T7). Mais il est probable que la même méthode pourrait être appliquée à toutes les superbactéries. Il reste encore un long chemin avant que ces recherches conduisent à de nouveaux traitements qui remplaceraient les antibiotiques ou leur permettraient de retrouver leur efficacité. Cette nouvelle approche offre d’immenses promesses, dans un domaine, où pour le moment, la recherche tardait à apporter des solutions.
Cendrine Barruyer et Esther Amar.
Publication dans PNAS, janvier 2015
—————————————–
* Déclaration de Michèle Rivasi, députée européenne, vice-présidente du Groupe Verts / ALE
Face à la montée de l’antibiorésistance, le retour de la thérapie par les bactériophages se précise en Europe
Lundi 8 juin 2015 s’est tenue à l’Agence européenne du médicament(1) la première réunion européenne sur la thérapie par les bactériophages, aussi connue sous le nom de phagothérapie. Acteurs académiques, industriels et politiques ont discuté des diverses façons d’encadrer cette thérapie prometteuse, notamment face à la montée de l’antibiorésistance.
Michèle Rivasi, députée européenne Vice-Présidente du groupe des Verts/ALE était présente à cette rencontre: » Cette pratique thérapeutique utilisant des virus cultivés dans le but d’affronter des bactéries précises a été inventée en France au début du XXe siècle mais curieusement abandonnée dans les années 1940 avec l’arrivée des antibiotiques. Elle s’est en revanche développée et maintenue jusqu’à aujourd’hui dans les pays de l’ancien bloc de l’est. En octobre 2013 j’avais fait adopter au Parlement européen un amendement(2) visant la réintroduction de la phagothérapie en Europe. Je me réjouis de voir que les choses bougent, la rencontre d’hier est une première étape.
Désormais, il nous faut donner un statut à ces virus tueurs de bactéries qui soignent mais qui ne sont pas des médicaments, et combler le vide juridique actuel qui les caractérise. Etant donné que les virus sont des organismes vivants, ils ne peuvent pas être brevetés, ce qui explique probablement le désintérêt qu’ils suscitent malheureusement au sein de l’industrie pharmaceutique. Par ailleurs, nous devons continuer les expérimentations afin de mieux connaître les vertus des virus, mettre au point des bonnes pratiques de laboratoire et assurer l’efficacité et la sécurité des traitements ainsi mis au point.
J’ai pu développer plusieurs propositions, notamment l’idée de financer des études cliniques sur les infections articulaires et de mettre en place une plateforme d’hôpitaux de référence parmi les Etats membres afin de développer ce type de thérapie . Une démarche de recherche est déjà en cours au niveau européen, il s’agit du projet Phagoburn (3) qui vise à développer un traitement par les virus des brûlures graves. Les résultats sont attendus pour la fin de l’année 2015. »
[:en]
New Tel Aviv University research introduces a promising new tool: a two-pronged system to combat this dangerous situation. It nukes antibiotic resistance in selected bacteria, and renders other bacteria more sensitive to antibiotics. The research, led by Prof. Udi Qimron of the Department of Clinical Microbiology and Immunology at TAU’s Sackler Faculty of Medicine, is based on bacterial viruses called phages, which transfer « edited » DNA into resistant bacteria to kill off resistant strains and make others more sensitive to antibiotics.
According to the researchers, the system, if ultimately applied to pathogens on hospital surfaces or medical personnel’s hands, could turn the tide on untreatable, often lethal bacterial infections. « Since there are only a few pathogens in hospitals that cause most of the antibiotic-resistance infections, we wish to specifically design appropriate sensitization treatments for each one of them, » Prof. Qimron says. « We will have to choose suitable combinations of DNA-delivering phages that would deliver the DNA into pathogens, and the suitable combination of ‘killing’ phages that could select the re-sensitized pathogens. »

Reprogramming the system
« Antibiotic-resistant pathogens constitute an increasing threat because antibiotics are designed to select resistant pathogens over sensitive ones, » Prof. Qimron says. « The injected DNA does two things: It eliminates the genes that cause resistance to antibiotics, and it confers protection against lethal phages.
« We managed to devise a way to restore antibiotic sensitivity to drug-resistant bacteria, and also prevent the transfer of genes that create that resistance among bacteria, » he continues.
Earlier research by Prof. Qimron revealed that bacteria could be sensitized to certain antibiotics — and that specific chemical agents could « choose » those bacteria more susceptible to antibiotics. His strategy harnesses the CRISPR-Cas system — a bacterial DNA-reprogramming system Prof. Qimron pioneered — as a tool to expand on established principles.
According to the researchers, « selective pressure » exerted by antibiotics renders most bacteria resistant to them — hence the epidemic of lethal resistant infections in hospitals. No counter-selection pressure for sensitization of antibiotics is currently available. Prof. Qimron’s strategy actually combats this pressure — selecting for the population of pathogens exhibiting antibiotic sensitivity.
« We believe that this strategy, in addition to disinfection, could significantly render infections once again treatable by antibiotics, » said Prof. Qimron.
Prof. Qimron and his team are now poised to apply the CRISPR/phage system on pseudomonas aeruginosa — one of the world’s most prevalent antibiotic-resistant pathogens involved in hospital-acquired infections — and to test whether bacterial sensitization works in a more complex microbial environment: the mouse cage.
Publication in PNAS, January 2015[:]