Hadassah (Jérusalem, Israël) : un cathétérisme cardiaque réussi sur un bébé prématuré de 860g

[:fr]
Pour la première fois en Israël, un cathétérisme cardiaque (vise à corriger différents types d’
Cette petite fille est née avec un trou béant dans l’aorte et la décision de lui appliquer un cathéter a rapidement été prise par l’équipe médicale, composée des cardiologues Sagui Gavri, Nurit Yaakobi et Gur Mainzer, ainsi que de la néonatologiste Noa Ofek.
Nurit Yaakobi, qui avait réalisé un fellowship en France grâce au soutien de Hadassah France et de ses donateurs, a souligné « l’importance de l’expérience acquise à l’Hôpital Necker à Paris » lors de cette opération.
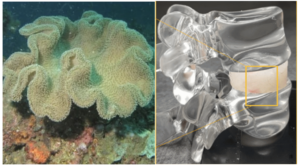
Cette procédure désigne l’insertion de longs tubes étroits dans les vaisseaux sanguins de la jambe pour atteindre le cœur et les artères afin d’y poser un bouchon vasculaire. Sans cette intervention, une opération chirurgicale complexe et risquée aurait dû être pratiquée.
Aujourd’hui, le nourrisson est en convalescence dans le service néonatal de soins intensifs du C.H.U. Hadassah Mont Scopus.
« Ce choix a été une véritable avancée pour notre équipe. Il nous permet maintenant de traiter en Israël de minuscules bébés prématurés souffrant de ce problème, ce qui leur évite une intervention chirurgicale particulièrement dangereuse », a déclaré le Dr. Mainzer.
[:en]
For the first time in Israel, a cardiac catheterization was successfully performed this week at Hadassah Hospital Ein Kerem on a fragile, premature infant weighing just under two pounds (860 grams).
Born four weeks ago together with her twin sister at Hadassah Hospital Mount Scopus, the tiny girl, weighing one pound, was delivered in the 26th week of pregnancy. When she gained a quarter pound, the procedure was scheduled.
She underwent a catheterization to close a central blood vessel. The large team was led by cardiologists Sagui Gavri, Nurit Yaakobi, and Gur Mainzer, as well as neonatologist Noa Ofek and anesthesiologist Shelly Stohl.
The baby’s condition is called PDA, patent ductus arteriosus, which means that the baby is born with an unclosed hole in the aorta. Before birth, blood doesn’t have to go to the lungs to be oxygenated. It goes through a hole that allows the blood to skip the circulation to the lungs. After birth, in a healthy heart, the blood must receive oxygen in the lungs, and the hole closes in the first few days after birth. Failure of the ductus to close is common in premature infants but rare in full-term babies.
Normally, the heart’s left side pumps blood only to the body, and the right side pumps blood only to the lungs. In a baby with PDA, extra blood gets pumped from the body artery (aorta) into the lung (pulmonary) arteries. This makes the heart and lungs work harder, and the lungs become congested. Catheters are used to close the PDA, but until now, this had never been done with such a premature baby in Israel.
The catheterization requires inserting long thin tubes into the blood vessels in the leg to reach the heart and the PDA. A vascular plug is inserted through the catheters into the PDA. Without catheterization, dangerous and complicated surgery must be done. “Tiny babies have a hard time recovering from surgery,” said Dr. Mainzer, director of the Pediatric Catheterization Unit at Hadassah.
The catheterization took the team four hours and was successful. The baby is now recovering in the neonatal intensive care unit at Hadassah Hospital Mount Scopus.
Dr. Yaakobi said the team has been acquiring the needed expertise at different hospitals and conferences around the world to be ready for the day when they would have to save a tiny premature baby with this heart defect.
“The catheterization was a breakthrough for our team, now allowing us in Israel to treat tiny premature babies who suffer from this problem, saving them from surgery,” said Dr. Mainzer.
[:]