TAU researcher harnesses targeted delivery of microRNAs to primary tumors in mice to block the movement of cancer

A new Tel Aviv University study finds that combining genetic therapy with chemotherapy delivered to a primary tumor site is extremely effective in preventing breast cancer metastasis.
The research was led by Dr. Noam Shomron of TAU’s Sackler School of Medicine in collaboration with Dr. Natalie Artzi of the Massachusetts Institute of Technology, and conducted by Dr. Shomron’s students Avital Gilam and Dr. Daphna Weissglas and Dr. Artzi’s student Dr. Joao Conde. Data on human genetics were provided by Prof. Eitan Friedman of TAU’s Sackler Faculty of Medicine and Chaim Sheba Medical Center.
Stopping cancer at the turning point
One in eight women worldwide are diagnosed with breast cancer during their lifetimes. Breast cancer is the second leading cause of cancer death in women. The chance that a woman will die from breast cancer is about 1 in 36. Early detection, while increasingly common, is not sufficient to preventing metastasis, the lethal movement of cancerous cells from a primary tumor site to colonies in vital organs. About 80 percent of women with metastatic cancer die from the disease within just five years of being diagnosed.
“The situation is bleak. Death rates from breast cancer remain high and relatively unchanged despite advances in medicine and technology,” said Dr. Shomron. “We wanted to find a way to stop metastasis from happening altogether. It’s the turning point, where survival rates drop exponentially.
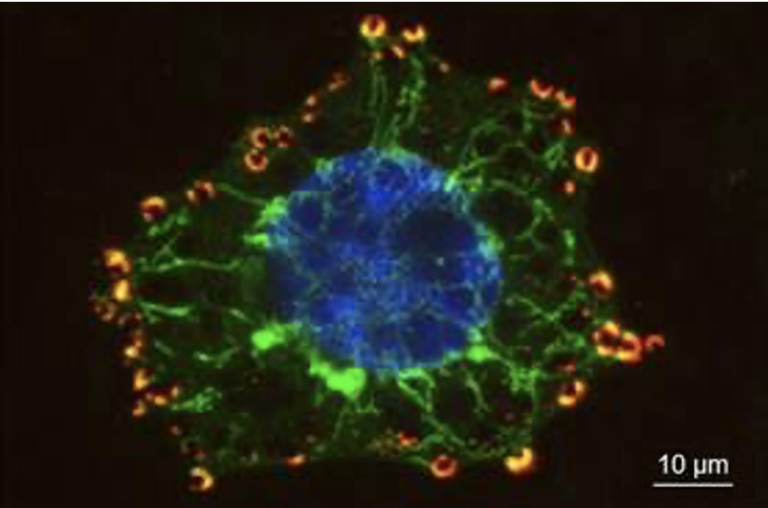
“Our mission was to block a cancer cell’s ability to change shape and move. Cancer cells alter their cytoskeleton structure in order to squeeze past other cells, enter blood vessels and ride along to their next stop: the lungs, the brain or other vital organs. We chose microRNAs as our naturally-occurring therapy, because they are master regulators of gene expression.”
Database, drugs and delivery
The researchers based their approach on the “3Ds” — database, drugs and delivery. The team began by exploring bioinformatics databases to investigate the span of mutations in a tumor and identify precisely which ones to target. The scientists then procured a naturally-occurring, RNA-based drug to control cell movement and created a safe nanovehicle with which to deliver the microRNA to the tumor site.
“We looked at mutations and polymorphisms that other researchers have ignored,” said Dr. Shomron. “Mutations in the three prime untranslated regions (UTRs) at the tail end of a gene are usually ignored because they aren’t situated within the coding region of the gene. We looked at the three UTR sites that play regulatory roles and noticed that mutations there were involved in metastasis.”
Two weeks after initiating cancer in the breasts of their mouse “patients,” the researchers injected into primary tumor sites a hydrogel that contained naturally occurring RNAs to target the movement of cancer cells from primary to secondary sites. Two days after this treatment, the primary breast tumors were excised.

The mice were evaluated three weeks later using CT imaging, flourescent labelling, biopsies and pathology. The researchers discovered that the mice that had been treated with two different microRNAs had very few or no metastatic sites, whereas the control group — injected with random scrambled RNAs — exhibited a fatal proliferation of metastatic sites.
From mice to humans
“We realized we had stopped breast cancer metastasis in a mouse model, and that these results might be applicable to humans,” said Dr. Shomron. “There is a strong correlation between the effect on the genes in mouse cells and the effect on the genes in human cells. Our results are especially encouraging because they have been repeated several times at TAU and at MIT by independent groups.”
The researchers are continuing their study of the effects of microRNAs on tumors within different microenvironments.
Publication in Nature Communications, 19/09/16