Tel Aviv University and DKFZ (Germany) discover the mechanism by which melanoma spreads to other organs in the body, and find ways to prevent the metastasis

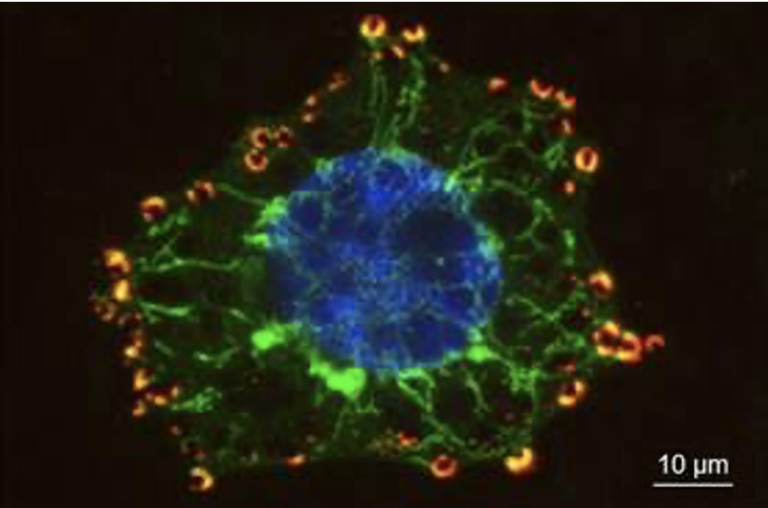
In a landmark discovery, researchers at Tel Aviv University have unraveled the metastatic mechanism of melanoma, the most aggressive of all skin cancers. The scientists discovered that before spreading to other organs, the tumor sends out tiny vesicles containing molecules of microRNA. These induce morphological changes in the dermis – in preparation for receiving and transporting the cancer cells. The researchers also found chemical substances that can stop the process, and are therefore promising drug candidates.
Melanoma, the most aggressive and lethal type of skin cancer, causes the death of one person every 52 minutes (according to data from the Skin Cancer Foundation), and the number of diagnosed cases has been on the rise for the past three decades. Despite a range of therapies developed over the years, there is still no full remedy for this life-threatening disease. A recent study at Tel Aviv University proposes new and effective methods for diagnosing and preventing this most deadly of skin cancers.
“The threat of melanoma is not in the initial tumor that appears on the skin, but rather in its metastasis – cancer cells sent off to colonize in vital organs like the brain, lungs, liver and bones,” says research leader Dr. Carmit Levy of the Department of Human Molecular Genetics and Biochemistry at Tel Aviv University’s Sackler School of Medicine. “We discovered how the cancer spreads to distant organs, and found ways to stop the process before the metastatic stage.”
Morphological changes in the dermis
The researchers began by examining pathology samples taken from melanoma patients, and the findings were striking indeed. “We looked at samples of early melanoma, before the invasive stage,” says Dr. Levy. “To our surprise we found changes that had never before been reported, in the morphology of the dermis – the inner layer of the skin. Our next task was to find out what these changes were, and how they related to melanoma.” In the ensuing long and complex study the group was able to discover – and also block – a central mechanism in the metastasis of melanoma.
According to Dr. Levy, scientists have known for years that melanoma forms in the outer layer of the skin, the epidermis. At this early stage the cancer is unable to send off colonizing cancer cells, because it has no access to blood vessels – the highways that carry the cells to other parts of the body. With no blood vessels present in the epidermis, the tumor first needs to contact the abundant blood vessels running through the dermis. But how is the connection made?
“We found that even before the cancer itself invades the dermis, it sends out tiny vesicles containing molecules of microRNA. These induce the morphological changes in the dermis, in preparation for receiving and transporting the cancer cells. It now became clear to us that by blocking the vesicles, we may be able to stop the disease altogether.”
Transforming melanoma into a nonthreatening illness
Having discovered the mechanism, the researchers proceeded to look for substances that could intervene and block the process in its earliest stages. They found two such chemicals: one (SB202190( inhibits the delivery of the vesicles from the melanoma tumor to the dermis; and the other (U0126) prevents the morphological changes in the dermis even after the arrival of the vesicles. Both substances were tested successfully in the lab, and may serve as promising candidates for future drugs. In addition, the changes in the dermis, as well as the vesicles themselves, can be used as powerful indicators for early diagnosis of melanoma.
“Our study is an important step on the road to a full remedy for the deadliest skin cancer,” says Dr. Levy. “We hope that our findings will help turn melanoma into a nonthreatening, easily curable disease.”
The group at Tel Aviv University worked in close collaboration with Prof. Jörg D. Hoheisel and Laureen Sander at the German Cancer Research Center (DKFZ) in Heidelberg, Dr. Shoshi Greenberger at the Sheba Medical Center and Dr. Ronen Brenner at the Wolfson Medical Center in Holon. Lab research was led by Dr. Shani Dror of Dr. Levy’s research group.
Publication in Nature Cell Biology, August 22th 2016